Opinion | 13 Confirmation Hearing Questions for Robert F. Kennedy Jr.
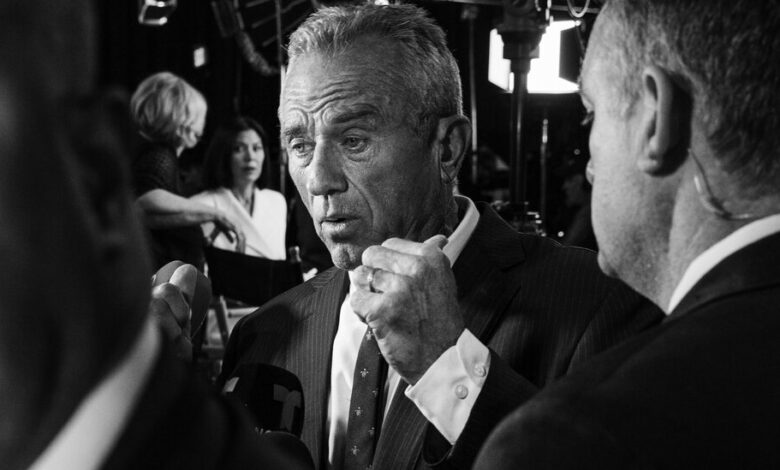
Perhaps never before has a nomination for health and human services secretary generated as much attention and divisiveness as that of Robert F. Kennedy Jr.
Times Opinion invited experts and leaders across disciplines and ideologies to share questions they believe Mr. Kennedy must answer before serving in a role that oversees a $1.7 trillion budget and wields enormous influence over drug approvals, public health and the nation’s research agenda. The questions reveal the stakes surrounding his nomination and offer a view of the broader fault lines in American health policy.
Vaccines
1. In 2019, Samoa experienced a devastating measles epidemic, resulting in nearly 2,000 hospitalizations and 83 deaths, mostly among children under age 4. During this crisis, Mr. Kennedy, you visited Samoa, promoted anti-vaccine misinformation through your organization, Children’s Health Defense, and met with anti-vaccine activists, undermining trust in public health leaders. These actions contributed to declining vaccination rates and delays in lifesaving M.M.R. vaccinations.
If confirmed as health secretary, you will bear responsibility for protecting vulnerable communities in the United States. If a vaccine-preventable outbreak happened here, how would you respond? — Dr. Nadine Tenn Salle, pediatrician and chief medical officer of the 2019 Hawaii medical response team to Samoa
2. You recently said that “if vaccines are working for somebody, I’m not going to take them away.” However, as health secretary, you could appoint individuals who might try to change the childhood vaccine schedule or weaken recommendations from the Advisory Committee on Immunization Practices, the group of experts that provides vaccine guidance to the Centers for Disease Control and Prevention. These recommendations shape insurance coverage and school entry requirements.
Will you now commit to not using this kind of soft recall where certain vaccines remain technically available but are no longer widely recommended or reimbursed by insurance, making them effectively inaccessible to much of the public? — Dr. Tom Frieden, former director of the C.D.C. and current chief executive of Resolve to Save Lives
3. You have a long record of vaccine skepticism — including having said repeatedly and recently that there’s “no vaccine” that is “safe and effective.” But you also recently said that you’re “all for” the polio vaccine and won’t take away anyone’s vaccines. Is this true? Which vaccines do you now believe to be safe and effective and what evidence changed your mind? — Kathleen Sebelius, former secretary of health and human services
Infectious diseases
4. Most presidents since Gerald Ford have faced an infectious disease emergency. Research has shown that trust, including in the government, is important in how well countries fare. We are facing a potential pandemic of H5N1 and whatever other unknowns Mother Nature sends our way. And yet, you have said you will tell National Institutes of Health scientists to take “a break” from studying infectious diseases for about eight years. How will you help the country develop and have confidence to use effective countermeasures if they are needed to control a pandemic? — Dr. Nicole Lurie, former assistant secretary for preparedness and response at H.H.S.
5. In your book “The Real Anthony Fauci” and in a recent interview with New York magazine, you suggested that H.I.V. isn’t the most likely cause of AIDS. You have suggested that lifestyle choices and the use of amyl nitrate may instead be to blame for the disease and that AIDS drugs may have caused “mass murder.” These views are scientifically baseless and dangerous.
Do you promise to support increased funding for and reauthorization of programs in the United States and around the world, such as the Ryan White Care Act and the President’s Emergency Plan for AIDS Relief, which have been critical in saving millions of lives and protecting millions of infants from H.I.V. infection? — Gregg Gonsalves, associate professor of epidemiology at the Yale School of Public Health and longtime AIDS activist
Food
6. Ultraprocessed foods account for nearly 70 percent of the American diet and have been linked not only to weight gain but also to a variety of chronic diseases. You’ve voiced strong criticisms of ultraprocessed foods. As health secretary, what regulatory steps, if any, are you prepared to take in order to curb their ubiquity? And would you consider proposing a tax on them? — Michael Pollan, journalist and author of numerous books on food, including “The Omnivore’s Dilemma”
Global health security
7. The search for Covid-19’s origin has revealed low visibility and minimal tracking of research that can cause pandemics. The new U.S. government policy to put guardrails on such research still leaves the door open for experiments that can inadvertently cause a pathogen to become more transmissible or deadly. How will you ensure that the United States is not continuing to fund risky research that can cause pandemics? — Alina Chan, molecular biologist and co-author of “Viral: The Search for the Origin of Covid-19”
8. The United States has always had a leadership role in global health and in the World Health Organization, whether it’s responding to outbreaks or developing and disseminating access to treatment or preventive measures like vaccines. If diseases are global, what is the United States supposed to do to protect its citizens without being a part of international organizations like the W.H.O.? — Dr. Helene D. Gayle, president emerita of Spelman College and former president and chief executive of the Chicago Community Trust
Health care
9. You’ve expressed skepticism over the use of GLP-1 drugs like Ozempic. Many people have found them enormously effective in helping them to lose weight when all else fails. Given that obesity can be a significant cause of chronic illness and early death, not to mention a huge financial burden on the health care system, this has been a welcome development. Unfortunately, it’s hard for many people to obtain these drugs. The drugs exemplify how high drug prices can drive unequal outcomes and strain the health system. What role do you see for emerging technologies in creating a more equitable and cost-effective health care system? — Dr. Aaron Carroll, pediatrician and president of the health policy organization AcademyHealth
10. Subsidies to help patients afford premiums for insurance plans purchased on the Affordable Care Act marketplaces are set to expire at the end of 2025. Enacted during the pandemic by the Biden administration, they have helped millions afford insurance, generally capping premium payments at 8.5 percent of income. If those subsidies are allowed to expire, premiums will jump by an average of 75 percent and will double for many, making coverage out of reach for millions of Americans. Will the new administration work to renew those subsidies, and if not, how does it intend to help Americans afford health care? — Dr. Elisabeth Rosenthal, physician and health care journalist
Abortion
11. Following the Supreme Court’s Dobbs decision, federal health agencies have found themselves at the center of the debate around abortion and contraception access. Do you believe agencies under your purview should restrict access to drugs such as mifepristone in states with laws limiting access to abortion? — M. Anthony Mills, director of the Center for Technology, Science and Energy at the American Enterprise Institute
12. During your independent campaign to be elected president, you said you supported limits on abortion after fetal viability. But fetal viability has changed as our medicine has improved. Sixty years ago, doctors often struggled to save babies born at 34 weeks, like your cousin Patrick Bouvier Kennedy. Today, some hospitals specialize in saving children born at 22 weeks. Does viability really indicate something about the limits of fetal personhood or just the limits of our technology and our empathy? — Leah Libresco Sargeant, journalist and author of “The Dignity of Dependence”
Health disparities
13. Rural and urban Americans have stark differences in life expectancy, health and health care access. Rural Americans live significantly shorter lives than urban Americans, with higher rates of death from accidents, cancer, cardiovascular disease and diabetes. Health conditions have consistently improved over the past 15 years in urban areas, but not in rural ones or among our tribal nations. This is often presented as a Republican versus Democratic issue — rural versus urban — but it’s really not about how Americans vote, but rather where they live.
What will you specifically do to address the health disparities of rural Americans, who for many diseases have survival rates as much as 15 percent to 30 percent lower than urban Americans? — Dr. Deborah Birx, former White House coronavirus response coordinator




